Before 1991, my family and I ate a fairly typical American diet. I tried to keep our meals as healthy as possible, limiting fat and calories (hello, fat-free Saltines), and ensuring we had plenty of protein (extra cheese on the pizza, please). Okay, clearly my understanding of nutrition back then was limited, but I had the best of intentions.
My entire world changed when my first child, Tyler, was about nine months old. He developed diarrhea, and as any first-time parent would, I raced him to the pediatrician, who calmly chalked it up to the antibiotics Ty was taking for ear infections. He assured me it would clear up within a week or so and invited me to return if it didn’t. And return, I did. Time and time again.
Every visit was the same. An obligatory look in the ears, nose, and throat, with the official I-attended-med-school-for-8-years-to-give-you-the-answer-you’re-waiting-for….“Hmmm… looks like he still has diarrhea,” the doctor declared with confidence. “But he’s had it for months,” I protested. “Shouldn’t it be clearing up by now?” “It should, and it will,” he assured me. “Just give it a little more time. He’s not dehydrated, and he’s still in the 75th percentile for height and weight, so there’s really nothing to worry about.” HE wasn’t the one changing 20 diarrhea diapers a day and doing several loads of laundry a day when the diapers weren’t able to hold everything in. He advised me to give him foods that would plug him up, like crackers and bread – and to call if it hadn’t cleared up in a few weeks. When I did call, I was informed that we would not be seen for Ty’s diarrhea. The sanctimonious receptionist informed me, “Our records indicate you’ve been in six times for diarrhea, and the doctor has explained to you that there is nothing to worry about. If you have a different concern, we can see you – but if you’re trying to make an appointment for the diarrhea, we must say no.” I was being fired from my pediatrics office.
Doctor number-two followed suit. A perfunctory look in the ears, nose, and throat, and a congratulatory declaration of, “You have a healthy baby boy.” “Healthy? He’s had diarrhea for months now. How is that healthy?” He glanced at his watch, aware that my five minutes was nearly up. Then Dr.-Do-Nothing actually took my hand in his and patted mine with a condescending, “Honey, mommies get really neurotic about diarrhea. Give it some time and let us know if it doesn’t clear up.”
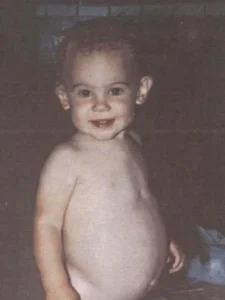
Patience is not my greatest strength. By now I was pregnant with number two, and between the hormones, the stress of having a sick baby, and running a business and a household, I was at wit’s end. I sought out a third pediatrician who sang me the same song: There’s nothing wrong with your baby. By this time, Ty’s belly had grown hugely distended, his arms and legs had wasted away to skinny little limbs, and his personality had transformed from a lively, energetic toddler to a cling, irritable, listless little boy. I figured I just had a quiet little boy who pooped a lot, and I gave up on trying to get to the bottom (so to speak) of his diarrhea.
When he developed an ear infection, we saw a fourth pediatrician – not for the diarrhea or huge belly and changed personality, because apparently those weren’t an issue. Since this doctor had never seen Ty before, we reviewed his medical history, and it was almost sheepishly that I mentioned the diarrhea and personality change. I felt a little silly complaining about something that was clearly not a problem. I mention that now not to illustrate how dumb I can be sometimes, but to exemplify how we can be intimidated by the medical system. These smart M.D.s tell you there’s nothing wrong with your kid – and three are in agreement – then there must be nothing wrong with your kid. But I digress….
This time there wasn’t the obligatory examination of the ears, nose, and throat. He said, “I know you’re here for an ear infection, and I’ll get to that in a minute. First, what’s going on with this belly?” as he thumped on it like it was a watermelon, making a hollow thudding noise. I could barely talk through the tears of gratitude. Finally someone was going to listen – someone was going to get to the bottom of it. And he did.
He sent us to Children’s Hospital in San Diego, where we saw a gastroenterologist who specialized in malabsorption conditions. It didn’t take long for him to let us know that he suspected a “rare, pediatric” condition called celiac disease (we know how that it’s neither rare nor a pediatric condition). Keep in mind this was in 1990. There were no blood or saliva tests available, and there was very little awareness of celiac disease other than among those who were specialists in malabsorption. The “test” back then started with an intestinal biopsy performed via endoscopy to examine the villi in the duodenum (I explain this in detail in my books and in other areas of this site). Once that baseline is obtained, we put him on a gluten-free diet for 4-6 months, and then we did a second biopsy. Presumably, the first biopsy would show blunted villi that are damaged due to gluten ingestion, and after being gluten-free for several months, the next biopsy should show villi returning to normal. Then we did a gluten challenge, putting him back on gluten for 3-4 months, followed by a third biopsy. As predicted, that third biopsy showed a deterioration in his villi because of the gluten challenge we had done. In 1991 it was confirmed: Tyler had celiac disease.
In my next blog post, “Our first days of being gluten-free (in 1991!),” I describe the terror I felt feeding my own son. “Give him one molecule of gluten, and it’s like giving him rat poison,” I was told. “I can handle that,” I mustered. “But what’s gluten?” “I don’t really know,” was the response I got from the pediatrician AND the hospital dietitian (who tried to assure me that I must mean he needs to avoid glucose, and I must have a diabetic child).
It was 1991 – there was no internet, there were no books or magazines dedicated to the subject, and I felt literally all alone and terrified to feed my son. But as terrified as I was, I knew that there was lemonade to be made. Finally we knew what was wrong with him – somehow having a diagnosis helps, even if it seems tough at first. While we knew there was no “cure” for celiac disease, we had the key to better health: a gluten-free diet. No medication, no surgery – simply a dietary modification (not to be confused with “a simple” dietary modification). I would do whatever it took to get my son healthy, and to ensure he had a happy, healthy future. It became my passion to help others do the same – I was a mom on a mission, and my future had forever changed.
